Menopause Monologues Part 1

Menopause Monologues Part 1
Menopause Monologues Part 1
Have you noticed yourself experiencing…
Anxiety and depression.
Hot flashes and night sweats.
Brain fog and exhaustion.
Unbeknownst weight gain.
You are not alone—these are all symptoms of perimenopause and menopause, and I’ve felt them too!
That’s why I invited my friend, fellow health coach, and Naturopathic Doctor, Stefania Tiveron, to join us for a series on these two critical and often overlooked seasons of life.
If you’re ready to take back your life and start making these experiences a little less miserable and a little more marvelous, this series will help you do it!
Take it away, Dr. Stefania!
What Menopause is…
Menopause is a natural progression of life. It represents a transition from fertility to age-related non-fertility. All healthy women will transition from this reproductive (premenopausal) period to a postmenopausal period marked by the cessation of menstruation, aka the end of your monthly cycle.
“The term ‘menopause’ specifically means the cessation of menstruation, and most often
occurs between the ages of 45 and 55 years, with the average age for the last period being 51 years.”
What Menopause is not…
Menopause is not a disease. It is often a time of increased opportunities and options! Given that it may compromise as much as half of a woman’s lifetime, this is a time when women have the greatest knowledge and opportunity for creativity, spirituality, and personal growth.
“In Traditional Chinese Medicine, menopause is seen as a time when women shift from a predominantly “yin” (passive, cool, moist, still, substance, dark) to predominantly “yang” (dominant, hot, dry, active, upward seeking, restless, productive) nature.
Often a time when women become more assertive, set boundaries, and pursue personal, academic and career goals.”
What’s happening in the body during Menopause, and what hormones are involved…
The onset of the menopausal transition is marked by changes in the menstrual cycle—from regular ovulation and cyclic menstrual bleeding to a period marked by amenorrhoea (lack of menses). This shift is often erratic early in the menopausal transition.
Menopause is defined after 12 months of continued amenorrhoea, or a combination of laboratory analysis showing elevated FSH (follicle-stimulating hormone) levels, plus 6 months of continued amenorrhoea. (FSH levels are associated with fertility. Increased levels are indicative of menopause.)
How your hormones change over time…
During perimenopause, the ovaries make DHEAs—Estrogen, Progesterone, and Testosterone. The adrenals (your glands) make DHEAs as well—which is the precursor for Estrogen, Progesterone, and Testosterone (systemically).
Postmenopause, the ovaries still make DHEAs and Testosterone, but stop producing Estrogen. The adrenals still make DHEAs as well, which is the precursor for Estrogen and Testosterone (locally).
The lack of estrogen and other hormones produced by the ovaries creates an estrogen deficiency and relatively higher androgen levels (ie. DHEAs and Testosterone). This hormonal shift contributes to common symptoms like hot flushes and night sweats.
Check out how these hormone changes happen over time in the chart below.
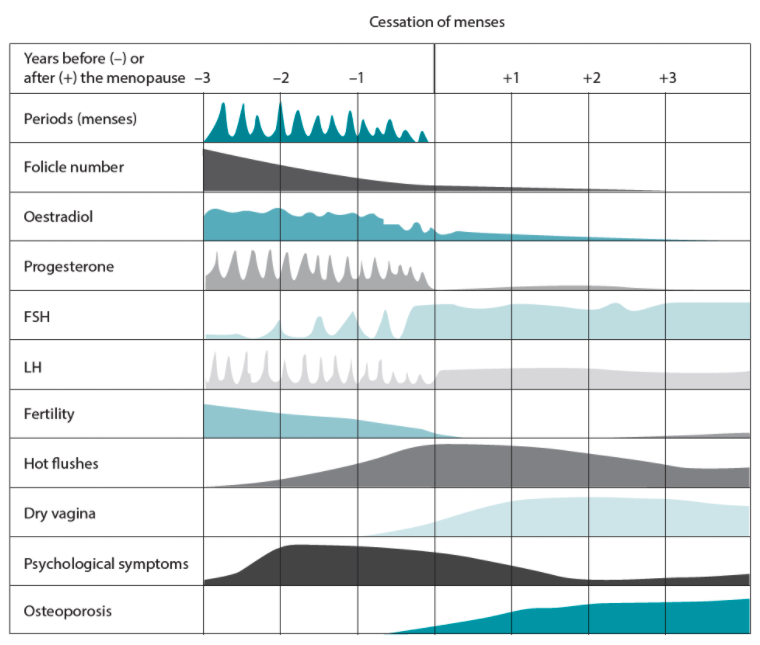
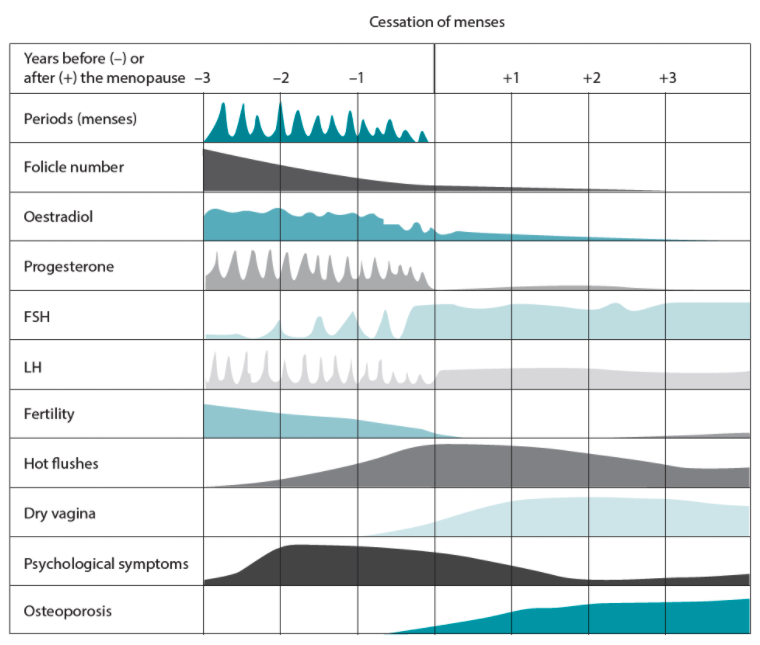
Source: John Wardle & Jerome Sarris. 2019. Clinical Naturopathy: An Evidence Based Guide to Practice, (Third Edition), 2019. Elsevier. Chp. 24 Menopause.
Here’s the CliffsNotes on Menopause:
-
-
- It’s defined after no period for 12 consecutive months or no period for 6 consecutive months and an elevated FSH (found in blood work).
-
-
-
-
Typically occurs in the late 40s to early 50s, and average age is 51 years.
-
-
-
-
-
Premature menopause occurs at age 40 or younger.
-
-
-
-
-
The term ‘perimenopause’ is most often used to describe the time leading up to and directly following menopause.
-
-
-
-
-
Eggs are no longer released.
-
-
-
-
-
Ovarian estrogen and progesterone production slows.
-
-
-
-
-
The ovaries continue to excrete minimal amounts of estrogen as well as significant amounts of androgens (DHEAs and Testosterone).
-
-
-
-
-
Sudden menopause can occur when the ovaries are removed (oophorectomy).
-
-
Women will experience the menopausal transition differently. Some women experience very little in the way of symptoms and/or intensity of symptoms. For others, this time is particularly debilitating.
A laboratory assessment of the following hormones may be used to assess risk factors and to tailor interventions according to individual needs based on your measurements of FSH, LH, Estrogen, Progesterone, TSH, Cortisol, DHEAs, Testosterone.
What are the adverse effects of Menopause?
Ann here again! I refer to these adverse side effects as “miserable symptoms” that can be dramatically improved through nutrition, movement, rest, self-care, hydration, and the right kind of exercise.
Here are some of the typical miserable symptoms one might experience during the menopause and sometimes perimenopause stage.
-
-
-
Hot flashes
-
-
-
-
-
Night sweats
-
-
-
-
-
Heart racing
-
-
-
-
-
Difficulty sleeping
-
-
-
-
-
Fatigue
-
-
-
-
-
Body aches
-
-
-
-
-
Headache
-
-
-
-
-
Migraine
-
-
-
-
-
Vaginal dryness
-
-
-
-
-
Vaginal infections
-
-
-
-
-
Low libido
-
-
-
-
-
Urinary incontinence
-
-
-
-
-
Bladder infections
-
-
-
-
-
Skin and hair issues (hair thinning, skin dryness, acne, facial hair)
-
-
-
-
-
Psychological symptoms (mood swings, anxiety)
-
-
-
-
-
Cognitive changes
-
-
-
-
-
Cardiovascular risk (the protective effects of estrogen on cardiovascular disease is no longer present)
-
-
-
-
-
Osteoporosis
-
-
Low estrogen levels also increase the risk of a number of other physical conditions, including osteoporosis and cardiovascular disease.
No fun, right?!
That’s why screening is a critical component to winning this season of your life!
Your baseline evaluation should be based on history, disease risks, current health problems, and family history. Please consult with your healthcare provider (HCP) about the following:
-
-
- Detailed personal medical history.
-
-
-
-
General physical examination.
-
-
-
-
-
Breast examination.
-
-
-
-
-
Pelvic examination.
-
-
-
-
-
Laboratory tests: complete blood count, blood chemistry, lipid panel, thyroid function panel, homocysteine, C-reactive protein.
-
-
-
-
-
Serum, Salivary and/or Urinary hormone testing: FSH, LH, Estrogen, Estrogen metabolites, Progesterone, TSH, Cortisol, DHEAs, Testosterone.
-
-
-
-
-
Screening mammography.
-
-
-
-
-
Bone density testing.
-
-
-
-
-
Cervical cytology (Pap smear).
-
-
-
-
-
Electrocardiogram.
-
-
-
-
-
Colonoscopy.
-
-
How do you offset the effects of Menopause?
There is considerable focus on the effects of hormone therapy (bioidentical and conventional) on menopausal symptoms and disease risks. However, other modifiable lifestyle factors such as exercise, cessation of smoking, weight loss, and reduced alcohol consumption are also associated with improved symptoms and decreased risk of disease.
Nutritional Considerations
Modify your diet to improve symptoms, and to reduce/prevent disease risk.
Focus on a diet rich in whole and unprocessed processed foods.
-
-
- Emphasis on vegetables, whole grains, beans, seeds, nuts, fruits, lean low-fat proteins, and healthful fats.
-
-
-
-
Follow the rainbow (the clean 15 vs. the dirty dozen)
-
-
-
-
-
Stay hydrated.
-
-
-
-
-
Reduce saturated fats and fried foods, simple carbohydrates, carbonated beverages, alcohol, sugar, and salt.
-
-
- Put down the vino and pick up the miso—or other beneficial nutrients.
-
-
- Avoid/reduce alcohol and caffeine, as both can worsen hot flashes.
-
-
-
- Avoid trigger foods, such as spicy food or fast food.
-
-
-
- Drink cold liquids during a hot flash.
-
-
-
- Increase consumption of Phyto-oestrogenic isoflavones found in foods and herbs. These compounds may mimic endogenous sex hormones and are associated with a reduction in vasomotor symptoms (frequency and intensity)
-
-
-
-
-
-
-
Foods: Miso, Milled flax, and tofu.
-
-
-
-
-
-
-
-
-
-
-
Herbs: Astragalus membranaceus and Scutellaria baicalensis (talk to your HCP).
-
-
-
-
-
- Increase your calcium and omega
-
-
- Introduce calcium-rich foods to decrease the risk of bone loss.
-
-
-
- Omega 3 fatty acids.
-
-
-
- Adequate calcium and vitamin D consumption are essential (a combination approach of food, supplements, and sunlight exposure may be required for Vitamin D levels).
-
-
Maintain a healthy heart.
-
-
-
Adverse cardiovascular risk is associated with type 2 diabetes, hypertension, and obesity.
-
-
-
-
-
Modifiable risk factors:
-
-
-
-
-
-
-
Focus on low glycemic index foods due to changes in insulin sensitivity.
-
-
-
-
-
-
-
-
-
Prioritize lean protein, high-fiber, and high-water vegetables, and healthy dietary fats.
-
-
-
-
-
-
-
-
-
Minimize saturated fats and fried foods, simple carbohydrates, alcohol, sugar, and salt.
-
-
-
-
-
Supplements (talk to your HCP first)
-
-
-
Collagen, Vitamins D and K2, broad-spectrum amino acids, L-glutamine, B-complex, Antioxidants, Omega 3 fatty acids, and Magnesium.
-
-
Movement Considerations
Movement and exercise can considerably improve your quality of life, reduce symptoms, manage stress, and support cardiovascular and bone health.
-
-
-
Choose enjoyable activities, and focus on movement. The more we move, the better our nutrition works for us!
-
-
-
-
-
Rest-based activity is key to balance and complement yang nature.
-
-
-
-
-
A combination of cardiovascular exercise and resistance training supports brain health, mental health, bone density, lean muscle mass, and fat loss.
-
-
- Regular exercise improves nutrient partitioning and body composition:
-
-
- More calories go toward muscle growth and/or energy provision.
-
-
-
- Fewer calories go to fat cells
-
-
Pelvic floor exercises encourage circulation and tone in genital areas which may improve:
-
-
- Sexual function and libido.
-
-
-
- Symptoms related to prolapsed organs and/or urinary incontinence. It is important to understand that your weight is merely a piece of data. While it can help you to assess how your weight management “plan” is working for you, there are many other ways to evaluate your progress or what changes may be of benefit.
-
Self-Care Considerations
Self-care is still important in your 40s and 50s. Emotionally and physically, this is a more challenging time due to hormonal changes. You and I both know at times, it’s hard to relax.
This is a beautiful opportunity to take control of your health and prepare for a new journey. How will you put yourself first?
Screening is key! Talk to your HCP about the best healthcare screens for you and your needs.
-
-
-
Stress management and new coping mechanisms. Meditation, low impact movement (yoga, pilates, walking), naps, building a sleep ritual, connection, prayer, time outdoors, gratitude practices, journaling. What is calling to you?
-
-
-
-
-
Sunlight exposure of 5–10 minutes per day may be required to boost Vitamin D production in the body.
-
-
-
-
-
Smoking and alcohol cessation/reduction.
-
-
-
-
-
Self-identity: This is a new chapter in your life, and an exciting time to reevaluate who you are.
-
-
Big shoutout to Dr. Stefania for teaching us what’s actually going on inside our bodies and equipping us with lifestyle tools that are proven to move the menopause needle from miserable to marvelous!
If you have questions for Dr. Stefania, leave them in the comments below, and we’ll be sure to respond with answers! If you want to learn more about Dr. Stefania, check out her website right here!
If you’re eager to learn more about menopause and ways to live more marvelously during that season, keep your eyes peeled for more on this series, or join my weekly newsletter, where I’ll be dropping exclusive content and more!
Article References
-
-
-
John Wardle & Jerome Sarris. 2019. Clinical Naturopathy: An Evidence-Based Guide to Practice (Third Edition), 2019. Elsevier. Chp. 24 Menopause.
-
-
-
-
-
Shelly Burns. Health Masters Live, 2019. Women’s Health Masterclass. Lesson 2 Perimenopause & Menopause. Accessed online.
-
-
-
-
-
Joseph E. Pizzorno, Michael T. Murray, Herb Joiner-Bey, The Clinician’s Handbook of Natural Medicine (Third Edition), 2016. Churchill Livingstone. Chp. 53 Menopause. Pages 624-647.
-
-
